22 Feb Patient diversity in clinical studies: The key to advancing precision medicine
By Emily K. pauli, Pharm.D.; Jeff Chen, MD/MBA; and Pelin Thorogood, M.Eng/MBA; Radicle Science via Clinical Leader
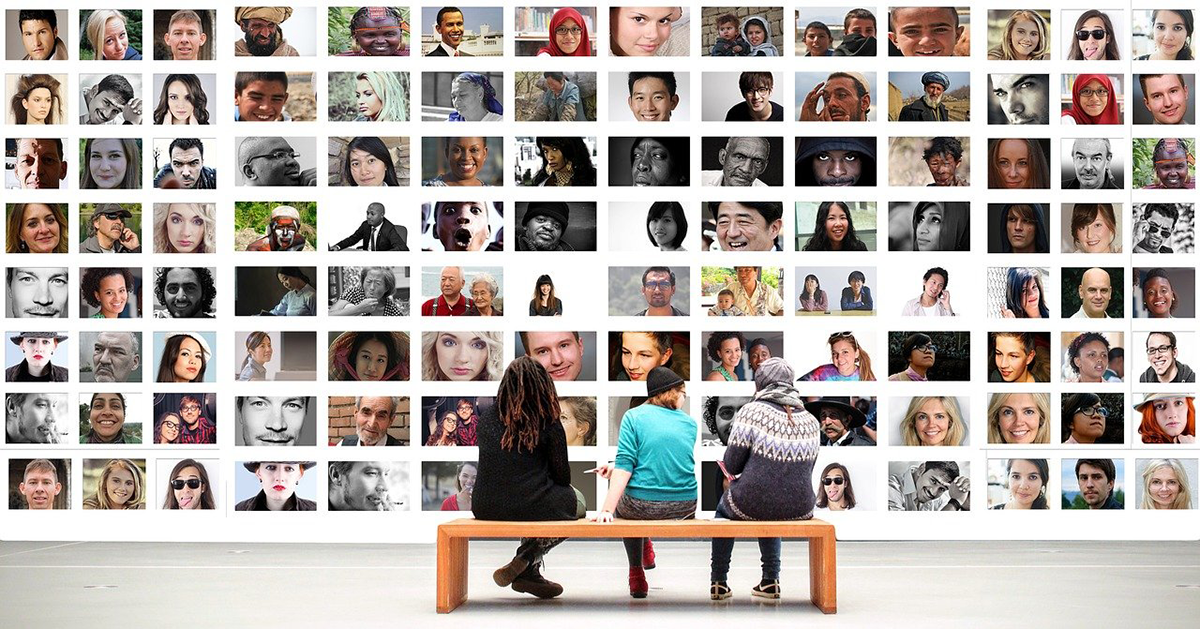
Precision medicine is about “delivering the right treatments, at the right time, every time to the right person,” as former President Obama aptly defined it. Large-scale longitudinal studies are necessary for precision medicine, but the constraints inherent to traditional clinical trials limit the understanding of key variables like gender, preexisting conditions, behavior, socioeconomics, race, and ethnicity.
Until we have better inclusion of participants with diverse demographics and behaviors – and can analyze that data in conjunction with prognostic data – we won’t know the effectiveness of a product for these large, underrepresented populations. Thankfully, crowdsourced virtual trials with intentional heterogeneity of participants are elegant solutions for getting us closer to precision medicine.
Heterogeneity is critical for precision care
Drug metabolism can differ across heterogeneous populations due to prognostic factors like age and gender, as well as allelic frequencies that tend to cluster by race/ethnicity. However, research often overlooks factors such as behavior and socioeconomic status. In a commentary in Nature, McCarthy and Birney argue that “clinical medicine must learn to develop more-holistic measures of individual risk, both genetic and non-genetic, and to combine these with clinical data over time to deliver better care.”
For medicine to become more precise, we must take into account all of the holistic data. As one example, numerous studies show genetics play a role in higher incidences of kidney disease among African Americans. This is why medicine uses more sensitive thresholds for screening and diagnosis of chronic kidney disease in African Americans, as “CKD progresses to end-stage renal disease far more rapidly in minority populations, with rates nearly four times higher in Black Americans than in white Americans.” However, there may be more at play here than alleles. “Socioeconomic factors and chronic stress, including the stress of racism, may increase the risk of having conditions that cause kidney disease — especially diabetes and high blood pressure.”
A holistic approach would give us invaluable insights that translate into precision care, and that’s precisely the approach the U.S. government is taking. The NIH is ambitiously combining both prognostic and demographic factors in a large-scale, intentionally heterogeneous, Big Data-driven study. The All of Us Research Program’s goal is to gather data from 1 million participants that reflect America’s diversity, especially from groups in biomedical research that have been underrepresented historically. The NIH believes: “Diversity in a research program is important for several reasons. First, where we live, how we live, and our background can all affect our health. Second, many groups of people have been left out of research in the past. This means researchers know less about their health.”
To advance medicine for all, we must advance research for all. As we increase diversity in our study populations, we expect to see differences in everything from health outcomes and adverse effects to consumption behavior. We also expect to see what’s unexpected, which is precisely why we need intentional heterogeneity in large-scale studies. Read more …



